Published on
By Jinghong Chen | Bond Life Sciences Center
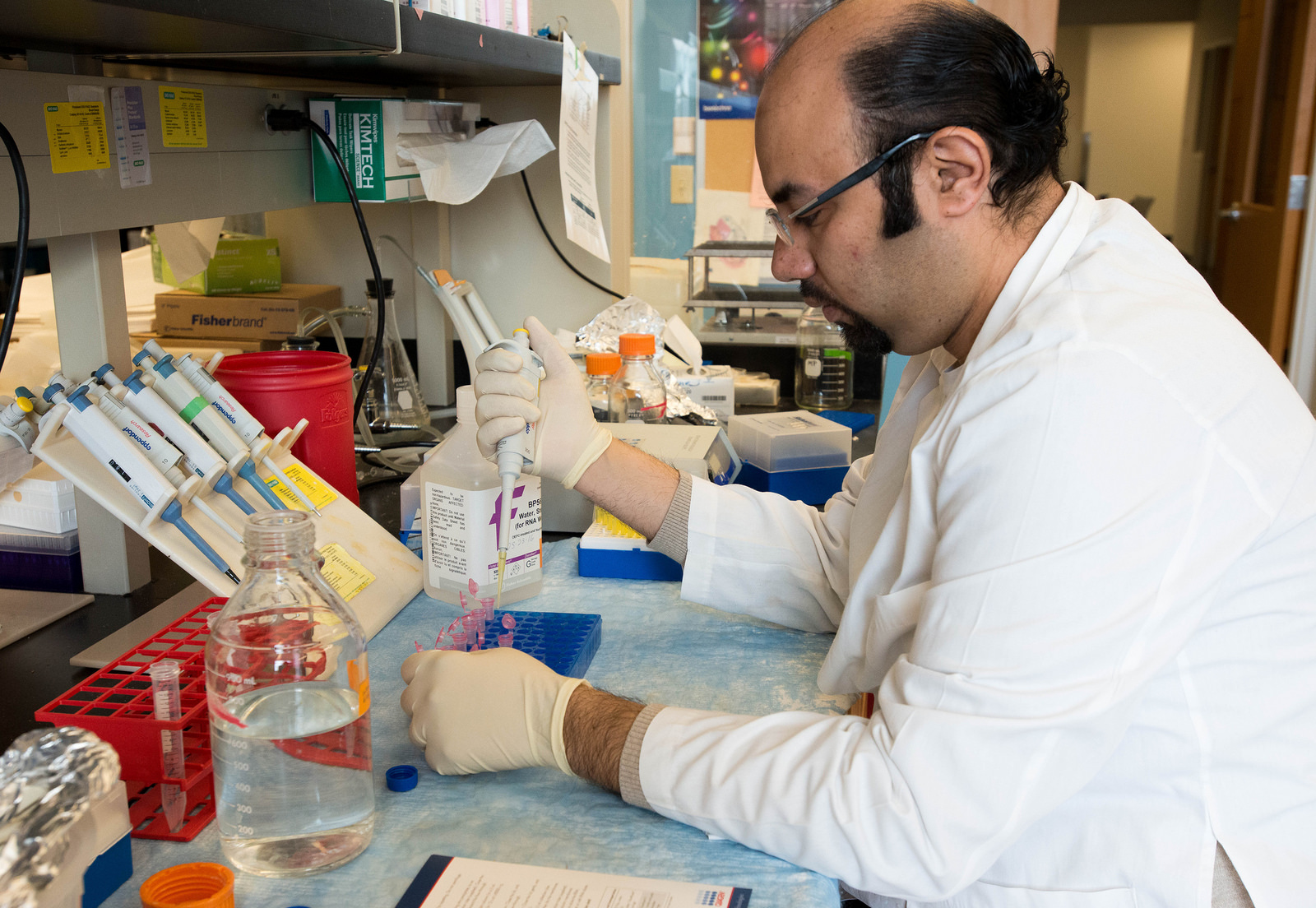
Mahmoud Khalafalla, a Ph.D. student at Weisman’s lab, is isolating RNA from salivary glands of Sjögren’s syndrome mouse model to look for the expression of pro-inflammatory genes. | photo by Jinghong Chen, Bond LSC
Our immune system is often the key to our health. Everyday, it works to protect us from foreign invaders such as bacteria and virus, but what happens when it attacks our own tissues?
Gary Weisman, a Curator’s Distinguished Professor of Biochemistry at the Bond Life Sciences Center, is working to advance our understanding of the mechanisms behind immune system function and autoimmune diseases such as Sjögren’s syndrome.
In our immune system, B cells are responsible for producing antibodies to recognize foreign invaders. However, in many autoimmune diseases, B cells produce autoantibodies that recognize our own proteins, causing inflammation and tissue damage. In Sjögren’s syndrome (SS), they attack the glands that produce saliva and tears.
Patients with SS often suffer chronic dry eyes and dry mouth, which might lead to bacterial infection, difficulties in swallowing and speech.
“The symptoms decrease the quality of life rather than the length of life,” said Lucas Woods, research lab manager in Weisman’s lab.
Although SS patients are at higher risk of developing lymphoma cancers and other concurrent autoimmune diseases that may increase mortality, Woods further explained.
According to the Sjögren’s Syndrome Foundation, there are an estimated four million people living with the disease in the U.S. For unknown reasons, 90 percent of them are female.
Yet, current clinical treatments only reduce symptoms by using artificial saliva and tears or cholinergic agents to promote fluid secretion, but there is no approved treatment to reduce the inflammation of the glands themselves. This is the focus of Weisman’s lab.
Sensor of danger
There are 15 different types of nucleotide receptors in humans that regulate numerous cell processes from inflammatory responses to tissue regeneration. Those receptors are stimulated by nucleotides such as ATP. In the past three and a half years, Mahmoud Khalafalla, a Ph.D. student in Weisman’s lab, has focused on one of them in particular – the P2X7 receptor.
Previous studies show increased P2X7 expression in salivary glands from SS patients, as compared to healthy individuals. To understand the reasons behind this, Weisman’s lab used genetically modified mice that develop disease traits similar to SS patients.
In this mouse model, Sjögren’s-like disease occurs when the immune cells invade salivary glands and damage the tissue, leading to decreased saliva production. The invasion of immune cells is triggered by proinflammatory cytokines, a type of signaling molecule that promotes the recruitment of immune cells to the inflamed areas.
But what induces those cytokines?
Weisman’s lab tries to piece together the answer. For the first time, they found that the P2X7 receptor is responsible for the release of these proinflammatory molecules from salivary gland epithelial cells.
To function, most cell-surface receptors require ligands that bind to the receptor to induce cellular responses. The ligand for the P2X7 receptor is ATP – the “energy currency inside of cells.” P2X7 receptors are activated when high concentrations of ATP are released to the outside of the cells, which typically occurs when the cells are injured during inflammation.
“P2X7 receptors [act like] the sensor of danger,” Khalafalla said.
After identifying the role of the P2X7 receptor, the lab then asked: if we stop its activation, what would happen?
Using a drug that inhibits P2X7 receptor activation, they blocked the receptor in their SS mouse model to determine its effect on the development of autoimmune disease. Interestingly, saliva secretion was restored when the P2X7 receptor is blocked while the levels of invading immune cells in salivary glands were dramatically reduced.
“This gives us the thought that [blockade of the] P2X7 receptor is really a promising strategy to reduce salivary inflammation. This may not only relate to Sjögren’s syndrome, but to other autoimmune diseases as well,” Khalafalla said.
Our receptor
Another similar receptor that plays a role in autoimmune diseases is the P2Y2 receptor, which has been referred to as “our receptor” by Weisman’s lab.
As one of the researchers who proved the existence of this receptor, Weisman has spent most of his career studying it.
One of his research projects investigating P2Y2 receptors in human disease recently gained a grant extension for another five years from the National Institutes of Health. The lab found that in a mouse model of SS, similar to the P2X7 receptor, the expression of P2Y2 receptors was increased in both the salivary gland epithelial cells and immune cells.
Furthermore, after they knocked out the P2Y2 receptor in the SS mouse model by breeding them with genetically-modified P2Y2 receptor knockout mice, the inflammation of salivary glands was dramatically reduced.
“The very next step is that we are going to isolate these immune cells out of the diseased mouse salivary glands, and characterize what kinds of cells they are. We want to know exactly which ones are controlling the development of autoimmune diseases, and how P2Y2 receptors and nucleotides like ATP in general are contributing to the diseases,” Woods said.
Gary Weisman is a Curator’s Distinguished Professor of Biochemistry at the Bond Life Sciences Center. His research focuses on the relationship between inflammatory diseases and nucleotide receptors. He currently works on a collaborative research project with Dr. Carisa Petris, an eye surgeon at the MU Hospital, to understand the mechanism of how Sjögren’s syndrome damages the tear-secreting lacrimal glands in mice.